Costs of diabetes complications: hospital-based care and absence from work for 392,200 people with type 2 diabetes and matched control participants in Sweden
Andersson E, Persson S, Hallén N, Ericsson Å, Thielke D, Lindgren P, Steen Carlsson K, Jendle J
Nation-wide Swedish study shows substantial societal costs of diabetes complications: Work absence twice as costly as hospital-based care.
The Swedish Institute for Health Economics publishes results from a nation-wide study on 392,200 people with type 2 diabetes and matched control participants in late September 2020 in Diabetologia.
The study is presented at the European Association for the Study of Diabetes, EASD, on 25 September 2020.
The rising number of people living with type 2 diabetes is a world-wide concern. Risk management preventing diabetes complications is the cornerstone of treatment of type 2 diabetes. Hospital care of diabetes complications has been pointed out as a major cost driver in studies on the economic burden of diabetes in Europe, the US and elsewhere. However, few data have been published covering multiple complications, their complex interactions, and the potentially long-term impact of diabetes complications on overall societal costs including work absence.
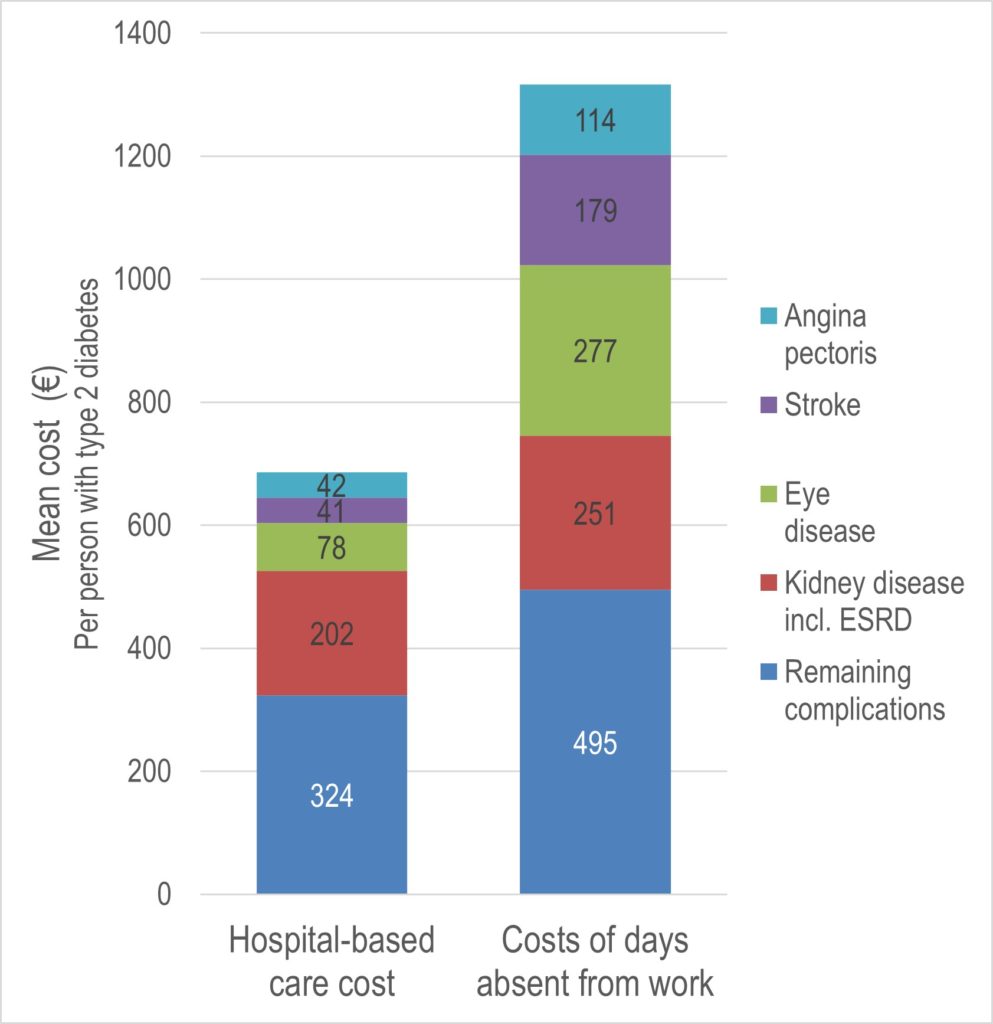
Results show substantial societal costs of diabetes complications. Importantly, costs of work absence related directly to diabetes complications were twice as high as costs of hospital-based care. The figure below illustrates the distribution of costs of diabetes complications in hospital-based care and from work absence as mean excess cost per person with type 2 diabetes compared to control participants in 2016. The excess cost of hospital-based care was €687 per person when averaging across all people with type 2 diabetes. The corresponding costs of days absent from work directly related to any of the studied complications nearly twice as high, € 1,317. More than half of these costs were caused by four key drivers of macrovascular and microvascular complications – kidney disease, eye disease, stroke, and angina pectoris.
The costs were derived from individual-level data for 392,200 people with type 2 diabetes and 1.6 million control participants. The study cross-linked national health data, social insurance, and socioeconomic administrative registers for the analyses. Costs of diabetes complications were estimated for year 2016 but presence of chronic complications was based on 20 years of retrospective data. The study is the largest of its kind covering multiple complications and their complex interactions in the analysis of hospital care use and work absence.
The authors conclude that consequences of diabetes complications and outcomes beyond those in the health sector must be considered both in the development of new treatments and in the development of policies and treatment guidelines.
Read more and download the article
Diabetologia, 2020
Published Online 24 September
DOI: https://doi.org/10.1007/s00125-020-05277-3